Defense Department award funds prostate cancer study
By Geri Clark
Weill Cornell Medicine researchers will receive a grant from the Department of Defense to conduct an in-depth study of the molecular machinery driving the most aggressive form of prostate cancer.
Most prostate cancers are a type called adenocarcinoma, which is regulated by the male hormone androgen. Advanced adenocarcinoma of the prostate is typically treated with drugs that cut off the supply of that hormone. Increasingly, however, these cancers are becoming resistant to androgen-blocking treatment and progressing to a more aggressive form of the disease, called neuroendocrine prostate cancer.
The grant, an Impact Award, will provide a Weill Cornell Medicine research team with three years of funding to identify patients who are at risk of developing neuroendocrine prostate cancer and to advance early treatment strategies to prevent that progression. The Department of Defense offers the Impact Award as part of its Prostate Cancer Research Program, which is dedicated to advancing scientific understanding of the disease with the goal of improving health outcomes.
“The neuroendocrine type of prostate cancer is associated with distinct molecular features,” said David Rickman, assistant professor of pathology and laboratory medicine at Weill Cornell Medicine and co-principal investigator of the Impact Award. “Understanding how it develops is critical for developing new treatment strategies.”
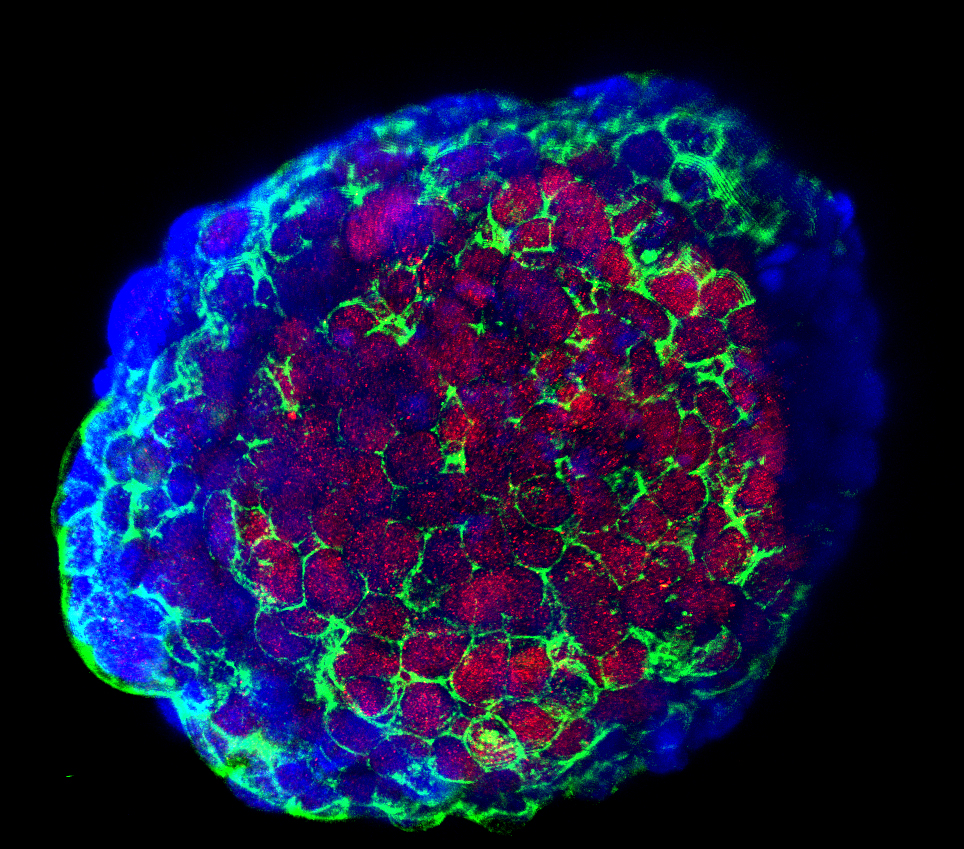
Rickman and Dr. Himisha Beltran, assistant professor of medicine at Weill Cornell Medicine and co-principal investigator of the Impact Award, will focus on one pathway, driven by a gene called N-Myc, which they have previously identified as a key driver of this cancer. Through earlier research in mice, the investigators discovered that prostate adenocarcinoma progresses to neuroendocrine prostate cancer when N-Myc is overactive. N-Myc also recruits a protein called EZH2 to help it activate the molecular machinery that causes this progression.
The investigators, both of whom are members of the Sandra and Edward Meyer Cancer Center and the Caryl and Israel Englander Institute for Precision Medicine at Weill Cornell Medicine, will employ clinical and preclinical approaches to their work. Beltran’s research will focus on using tumor samples from patients to identify how and when N-Myc drives the cancer and the disease’s response to treatment. Rickman will create a mouse model to better understand how N-Myc works and to test new treatment options. “It is team science,” Beltran said. “We will work together to better understand the pathogenesis and molecular biology of neuroendocrine prostate cancer by integrating preclinical modeling with patients’ clinical and molecular features.”
At the end of three years, the researchers hope to have developed innovative treatment strategies that can be applied directly to patients. “There are several unanswered questions about this cancer,” Beltran said. “We hope to get some answers that can help patients.”
Geri Clark is a freelance writer for Weill Cornell Medicine.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe