Scientists sequence genome of classical Hodgkin lymphoma
By Abigail Fagan
A team of researchers has sequenced the genome of classical Hodgkin lymphoma, illuminating exactly which proteins are altered in individual patients. The findings could pave the way to delivering personalized treatments and more effective options, since current treatments can be toxic and don’t work for nearly 20 percent of patients diagnosed with the disease.
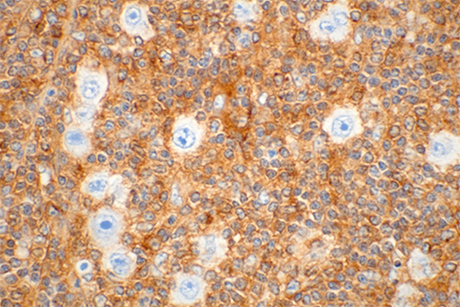
In the study, published Dec. 8 and as a plenary paper in the Feb. 12 issue of Blood, researchers sequenced the genomes of 10 different patients, creating a catalog of mutations in the harmful Reed-Sternberg cells that characterize classical Hodgkin lymphoma (cHL). Armed with this information, scientists can develop drugs that target these specific alterations to compensate for what has gone awry.
“Now we have a better idea of what mutations there are, and going forward therapies can be adapted to specific patient populations according to their genomic composition,” said senior author Dr. Ethel Cesarman, professor of pathology and laboratory medicine at Weill Cornell Medical College.
Although scientists have sequenced the genomes of many other diseases, the cHL genome has remained elusive due to the difficulty of isolating Reed-Sternberg cells, which usually comprise less than 1 percent of a total cHL tumor. The team employed a technique that separates larger cells and looks at the proteins on their surface, called fluorescence-activated cell sorting, to isolate the Reed-Sternberg cells and sequence the cancer genome, said senior author Dr. Mikhail Roshal, a pathologist at Memorial Sloan Kettering Cancer Center.
Once the researchers could see the genes of the cancerous cells, they examined the data for trends. About two-thirds of patients had mutations in the protein Beta-2-microglobulin, which make the Reed-Sternberg cells hide from the immune system. Patients with this mutation actually have a fairly positive prognosis, with nearly an 80 percent likelihood of being cured. Though their outcomes may originate in their typically younger ages – the median age of patients with this mutation is 30, compared with 47 for those without it – and tumor subtype, which is less aggressive than other forms of Hodgkin, understanding this common mutation allows scientists to continue improving existing medications, perhaps by reducing the dosage, Cesarman said.
Working with graduate student and first author Jonathan Reichel, Cesarman and Roshal also discovered other mutations in the cells that already have been cataloged, studied or have a corresponding treatment in other cancers. In these cases, doctors can sequence a cHL patient’s tumor (which is already common practice for other cancers and now feasible for cHL), identify their altered gene, and provide an effective corresponding treatment.
“Being able to sort and purify these cells was a breakthrough,” Cesarman said. “Knowing the genomics can eventually help to personalize treatment for these patients.”
Abigail Fagan is a freelance writer for Weill Cornell Medical College.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe