Protein networks help identify new chemo drug candidates
By Geri Clark
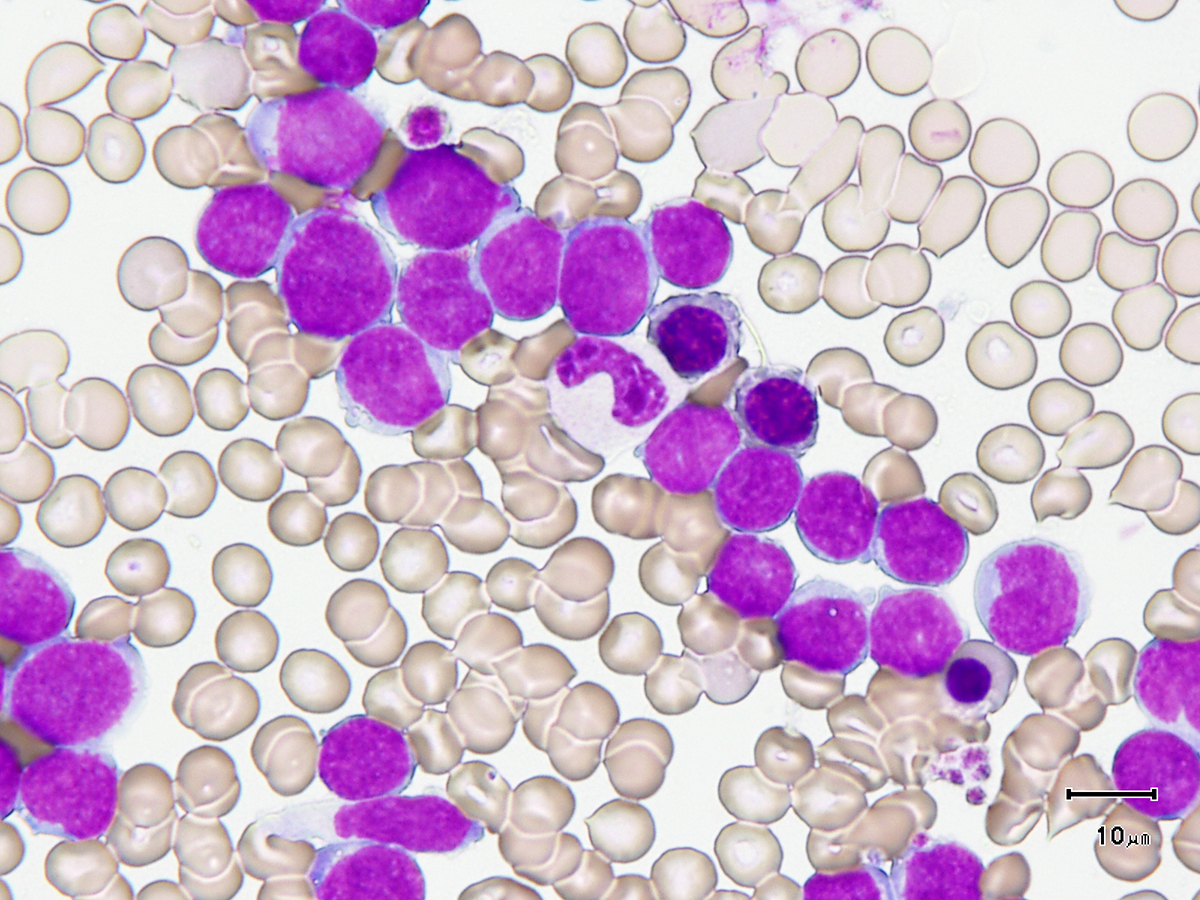
An experimental chemotherapy kills leukemia cells that are abundant in proteins critical to cancer growth, according to new research from Weill Cornell Medicine.
The findings may offer scientists a new biomarker to pinpoint patients with an aggressive form of the blood cancer who will most likely respond to the treatment.
In the study, published Nov. 25 in Cell Reports, the investigators focused on a drug developed by Dr. Gabriela Chiosis at Memorial Sloan Kettering Cancer Center called PU-H71. The drug targets a tumor-enriched form of the protein teHSP90, which is critical to the growth of cancer cells. Without this protein, the cells cannot survive.
However, earlier tests in acute myeloid leukemia, an aggressive cancer in which the bone marrow makes abnormal blood cells, had shown that PU-H71 only killed some leukemia cells.
“We observed that only a subset of leukemia patient samples were sensitive to the drug,” said co-senior author Dr. Monica Guzman, assistant professor of pharmacology in medicine in the Division of Hematology and Medical Oncology at Weill Cornell Medicine. “We wanted to be able to identify which patients with leukemia would respond to this drug.”
The research team, which included Dr. Gail Roboz, director of the Leukemia Program and professor of medicine at Weill Cornell Medicine, and other collaborators from Memorial Sloan Kettering and the University of Rochester, focused on groups of proteins that function within signaling networks in leukemia cells. These networks are critical for survival of acute myeloid leukemia cells, which in turn are dependent on teHSP90.
The researchers identified two of these networks that were important for cancer cells to function. They treated the leukemia cells with PU-H71 and found that the drug killed cells with high levels of these protein-signaling networks. Cells with less active signaling networks did not respond to PU-H71.
“Higher activation of these networks makes the leukemia cells more dependent on Hsp90,” Guzman said. “Since PU-H71 targets teHsp90, leukemia samples with these features are good targets for treatment with the drug.”
The next step for Guzman’s team is to test their findings in patients, most of whom are older adults. Even with treatment, the five-year survival rate is only about 25 percent; investigators believe that this is because there is great variation in the biology of acute myeloid leukemia, but not in treatments for the disease.
“We are working on a tool that will quickly and easily identify patients whose cancers will respond to PU-H71,” she said. “We are really looking forward to seeing this in leukemic patients and being able to offer them a new treatment.”
Geri Clark is a freelance writer for Weill Cornell Medicine.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe