Cancer cells' ability to self-repair may spawn new treatments
By Tom Fleischman
Because they have narrow bodies and no collarbones, mice are able to squeeze through holes as small as a quarter-inch in diameter.
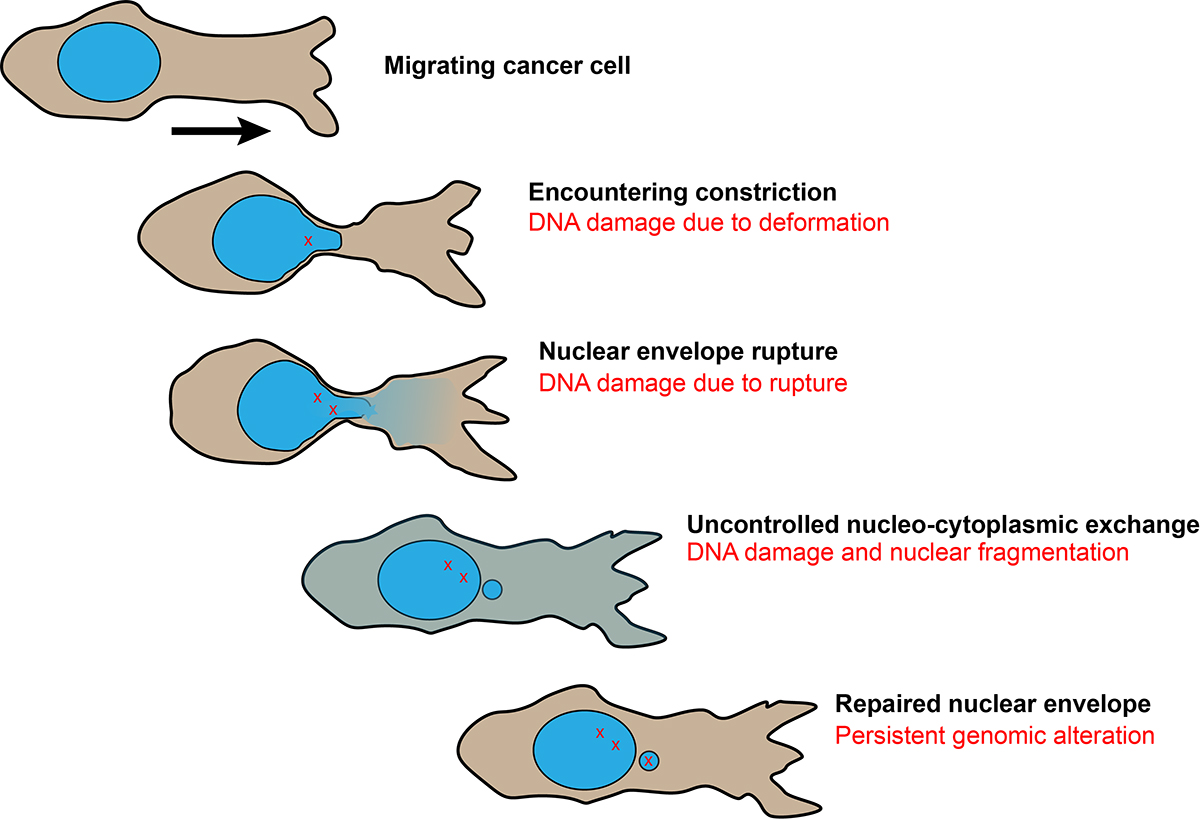
Cancer cells similarly are able to migrate through extremely tight quarters but with a major difference: The journey often comes at a price – the deformation and, in some cases, rupture of the outer lining of a cell’s nucleus.
A research group headed by Jan Lammerding, associate professor of biomedical engineering, has been studying this phenomenon in hope of using it to develop both treatment and diagnostic solutions for the millions of people who deal with cancer every day.
Lammerding’s group reports on this research in a paper published online March 24 in First Release, from the journal Science. His group’s paper is being published simultaneously with research by a French group, which found similar results in immune cells.
While deformation and rupture can sometimes lead to apoptosis (cell death), the cell also has the ability to repair itself.
“I think most cell biologists would probably say that these cells will not do very well after deformation and rupture,” said group member Philipp Isermann, a visiting scholar in biomedical engineering. “And it was quite surprising that about 90 percent of these ruptured cells survived.”
Added post-doctoral researcher Celine Denais: “You would think that, as with a balloon, at some point it will pop. We’ve been amazed with how these cells can handle this deformation.”
There is also the possibility that a ruptured cell could mutate into a more aggressive form of cancer.
“You have so many migrating cells,” Lammerding said, “that even if a small fraction of them picks up a mutation, that is bad because it means the cancer is evolving.
“The good part is, this rupturing also makes the cancer cell vulnerable,” he said. “Most cells in the body stay in place, and it’s presumably mostly cancer cells that are moving around. So if we can block the mechanisms that allow them to repair themselves, then we potentially could target metastatic cancer cells.”
Lammerding began his work in this area while teaching at Harvard Medical School. Part of the reason he came to Cornell in 2011, he said, was to take advantage of the fabrication capabilities at the Cornell NanoScale Science and Technology Facility, where the model environments used in the study were built.
“They work very well and have become very popular,” he said. “Every time I go to a meeting and present this work, people come up to me and say, ‘Can we get some of these models?’”
The group looked at two factors in the cell’s migration process: the rupturing of the nuclear envelope, which they tracked using green and red fluorescent proteins normally localized to the cell nuclei, but that spill into the cell body when the nucleus ruptures; and damage to the cell’s DNA.
“We’re still trying to find out if there are differences between cells, and a lot of what we see is very similar between normal cells and cancer cells,” he said, adding that by trying to identify potentially unique deformation-and-repair properties of cancer cells, treatments that are minimally deleterious to healthy cells may be developed.
“Now that we kind of know what we’re looking for, now that we know the molecular pathways involved in the repair,” he said, “could we then specifically target invasive cancer cells and not have the sledgehammer that hits everything?”
Other contributors to the paper, “Nuclear envelope rupture and repair during cancer cell migration,” included: Rachel Gilbert, former undergraduate and master’s student in biological engineering; Alexandra McGregor, Cornell graduate student in biomedical engineering; and former postdoctoral fellow Patricia Davidson, now at the Institut Curie in Paris. The group was also assisted with in vitro and in vivo experimentation by Katarina Wolf and Peter Friedl of Radboud University Medical Center in the Netherlands.
This work was supported by grants from the National Institutes of Health, the Department of Defense Breast Cancer Research Program, the National Cancer Institute and the National Science Foundation.
Media Contact
Get Cornell news delivered right to your inbox.
Subscribe